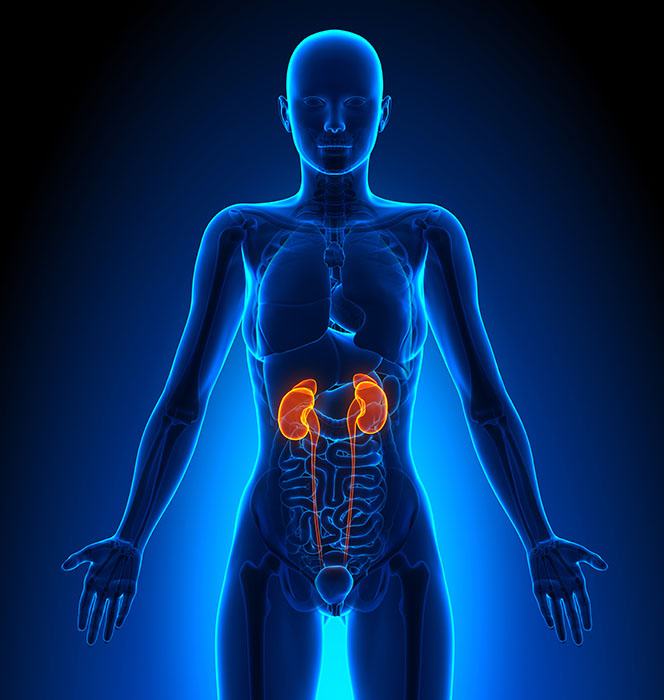
The function of the kidneys
Kidneys are two bean-shaped organs, weighing about 160 g each and are located on either side of the backbone under the ribcage. They play an essential role in your health as they are your blood’s filters!
The main function of the kidneys is to continuously remove toxins (produced by your body’s
metabolism and the digestion of food) and to regulate the quantity of water and minerals in your body (with urine as the resulting waste). They also contribute to the regulation of your blood pressure and to the production of red blood cells and vitamin D(1).
Progressively, your kidneys will lose some of their efficiency. In particular, the kidneys’ ability for removal of toxins and excess water will not function properly anymore.
Causes and symptoms
There are many symptoms of kidney disease (e.g. fatigue, insomnia, lack of appetite,
nausea…) and they vary considerably from one patient to another. Some people do not
notice any symptoms at all (which is why this is sometimes referred to as a “silent disease”).
Diabetes and hypertension are the most frequent causes of renal failure.
Through their different mechanisms, these pathologies affect the blood vessels of the
kidney and cause deterioration of the functioning part of the organ.
Other causes of renal failure can be genetic predisposition, the development of kidney stones,
chronic inflammation, or toxic substances(2) …
End-stage chronic renal failure is not a rare disease. Its frequency increases with age,
especially after 65.
• Over 2 million people worldwide currently have end-stage chronic renal failure (i.e. patients
receiving treatment or having received a kidney transplant)(3). The number of people suffering from this disease is likely to increase further in the years ahead as a result of the ageing population and an increase in diabetes.
The treatment choice
The purifying function of the kidneys is vital. At the end-stage of renal failure it is essential to replace this function through an appropriate treatment.
• During your pre-dialysis consultation, the medical team will suggest different renal replacement options: kidney transplant, in-centre haemodialysis or home dialysis.
Two major techniques exist for dialysis at home: peritoneal dialysis and home haemodialysis.
• Deciding the type of treatment that fits in best with your way of life is your personal choice, taking into account your own lifestyle and your professional and family priorities. Careful consideration allows you to take an active role in your therapy choice in order to preserve your quality of daily life.
KIDNEY TRANSPLANT
Tissue compatibility is ensured to reduce the risk of rejection of the transplanted organ. The risk exists nevertheless and for this reason an anti-rejection treatment is prescribed.
A transplant is the treatment option that will give you the closest to a normal life.
Registration on the waiting list for a transplant depends on your overall health, which is
assessed during a detailed medical examination. This is the responsibility of your referring
physician(4).
HOME DIALYSIS
> PERITONEAL DIALYSIS
This treatment mode makes use of a natural membrane, the peritoneum, which lines the abdominal wall. This membrane contains a large number of blood vessels.
When in contact with dialysis fluid, introduced into the abdomen through a flexible tube (a permanent catheter), this membrane acts as a filter to rid your blood of the waste matter that your kidneys are no longer able to remove.
• Continuous ambulatory peritoneal dialysis (CAPD) is a manual technique carried out during the day. The process introduces a quantity of dialysis fluid via the catheter 3 or 4 times a day, then empties the fluid after 4 to 6 hours of dwell time, during which time the particle exchange has taken place.
• In Automated Peritoneal Dialysis mode (APD), the renewal of the dialysis fluid is
carried out automatically by an apparatus (the cycler) connected to your catheter
during the night. The duration of treatment varies between 8 and 12 hours(5).
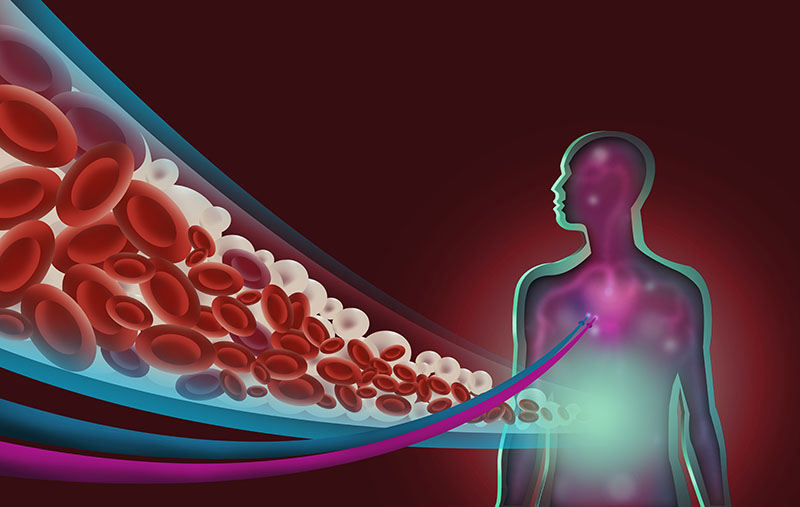
> HOME HAEMODIALYSIS
Haemodialysis is the most frequently used technique, both at home and in dialysis centres. It works by taking the blood through a circuit outside the body, purifying the blood as it passes through a device known as an “artificial kidney” – dialyser – before returning it to the body.
This circuit outside the body usually starts from an access area in the arm called an “arteriovenous fistula”. A device called a “dialysis monitor” controls the flow of blood and dialysis fluid: this is the fluid that allows the removal of toxins by particle transfer through the dialyser membrane.
The latest monitors, which are compact and user-friendly, make this technique perfectly safe in the home environment. This equipment allows short daily treatment,
offering a more physiological therapy that is easier to tolerate for the patient.
Daily haemodialysis is easy to integrate into your daily life and offers an advantage in terms of quality of life and independence.
• Before confirming the choice of home haemodialysis, the home dialysis team assesses your life plan, your motivation to carry out the treatment autonomously, and the feasibility of the technique with thought regarding your family environment or the suitability of your home.
IN-CENTRE HAEMODIALYSIS
• In the self-care haemodialysis unit, the nephrologist is not present and you take an active role in your treatment, retaining your autonomy.
• The haemodialysis centre is there to help patients with a more complicated pathology. A complete medical team is on-hand to take care of the dialysis session.
At all of these types of dialysis facility, the sessions are usually carried out three times a week. The duration of each session is approximately 4 hours.

Home haemodialysis
Recent technological innovations (miniaturization, no water treatment, performance) have allowed the consideration of home haemodialysis as a real option. Occurring more frequently (generally daily) with shorter sessions (2 hours- 2 hours 30) daily home haemodialysis provides a considerable advantage in terms of quality of life and reduction of complications, in particular cardio-vascular stress.(8)
This therapy allows foreseeing a more independent future, without the constraints of in-centre haemodialysis (fixed schedules, travel, long dialysis sessions)(8).
The role of the family and the care partner
Whatever the therapy choice, your family and relatives play an important role to accompany you and support you on a daily basis. Their life is also impacted – daily activities, home, holidays – and the therapeutic choice should be done with a common agreement between you, the patient, your family and the nephrologist. Even though home dialysis therapies become more and more user-friendly, family members should share this choice, and then the therapeutic benefit and well-being become profitable for all the family.
